“I can love just like you,
I can dance just like you,
I can run just like you,
and more importantly – I can work just like you.
Yet, all I wish is if I could make red blood – just like you.”
Thalassemia is not just a long medical word. It’s a serious inherited blood disorder in which the body fails to produce enough healthy red blood cells. For someone born with Thalassemia Major, this means they need regular blood transfusions to survive, often every two to three weeks, starting from early childhood.
But blood alone isn’t enough.
Those frequent transfusions cause excess iron to build up in the body, which can damage the heart, liver, and other organs. That’s why patients also need daily medication called chelation therapy to remove the excess iron and keep their bodies safe.
Now here’s the tougher part: while all of this sounds routine on paper, it’s not so easy in real life. Access to safe blood, reliable chelation medicines, trained specialists, and regular monitoring is a challenge for many families, especially those from lower-income backgrounds. And unfortunately, without consistent care, complications pile up quickly.
Thalassemia is manageable and even curable in some* cases; when there is proper awareness, timely support, and access to care. That’s what we’re here to fight for.
Treating Thalassemia is not a one-time thing. It’s a lifelong journey, and it’s different for every warrior.
It usually involves:
This is the first and most essential step in Thalassemia care. For most Thalassemia Major patients, regular blood transfusions are non negotiable.
To stay healthy and active, patients need to maintain a pre transfusion hemoglobin level of around 9 to 10.5 g/dL, which is considered optimal. This usually means getting blood transfusions every 15 to 20 days, sometimes every 2 to 3 weeks, depending on the individual’s body and condition.
Being adequately transfused helps children grow better, supports normal activity levels, and reduces complications. But it also means frequent hospital visits and a continuous need for safe, well screened blood, which is still a challenge in many parts of the country.
Chelation therapy usually begins after 10 to 20 blood transfusions, or when a child is around 2 to 3 years old, once iron levels in the body start rising.
With repeated transfusions, excess iron begins to accumulate in vital organs like the heart, liver, and endocrine glands. When ferritin levels rise above 1,000 ng/mL, iron overload becomes harmful and needs active management.
Chelation is a daily medication that removes this extra iron and keeps the body optimally chelated. Skipping chelation is not an option, because iron damage builds silently. Sadly, many families either struggle to afford chelation medicines or are not fully aware of how critical they are for long term survival.
Thalassemia is not just a blood disorder. Over time, it can affect growth, hormones, bones, immunity, and emotional well being. That is why treatment goes far beyond transfusions and medicines.
Regular follow ups with hematologists, endocrinologists, cardiologists, and psychologists are crucial. Hormone levels, bone health, heart function, and mental health all need close attention, especially during teenage years and early adulthood.
When all these specialists work together, it becomes holistic care, addressing not just survival, but quality of life for a Thalassemia patient.
A Bone Marrow Transplant is currently the only established cure for Thalassemia. It works by replacing the faulty blood forming system with healthy stem cells from a matching donor.
While BMT can be life changing, it comes with challenges. Finding a suitable donor is not always easy, the procedure is expensive, and it requires strong medical infrastructure and long term follow up. Because of these barriers, BMT is still not accessible to many families.
In recent years, research in gene therapy and gene modification has shown promising progress. This approach focuses on correcting or modifying the faulty gene responsible for Thalassemia, so the body can produce healthy hemoglobin on its own.
While still expensive and available only in limited settings, gene therapy is emerging as a probable future cure or long term treatment option for Thalassemia Major. As research advances and access improves, it brings new hope to families worldwide.
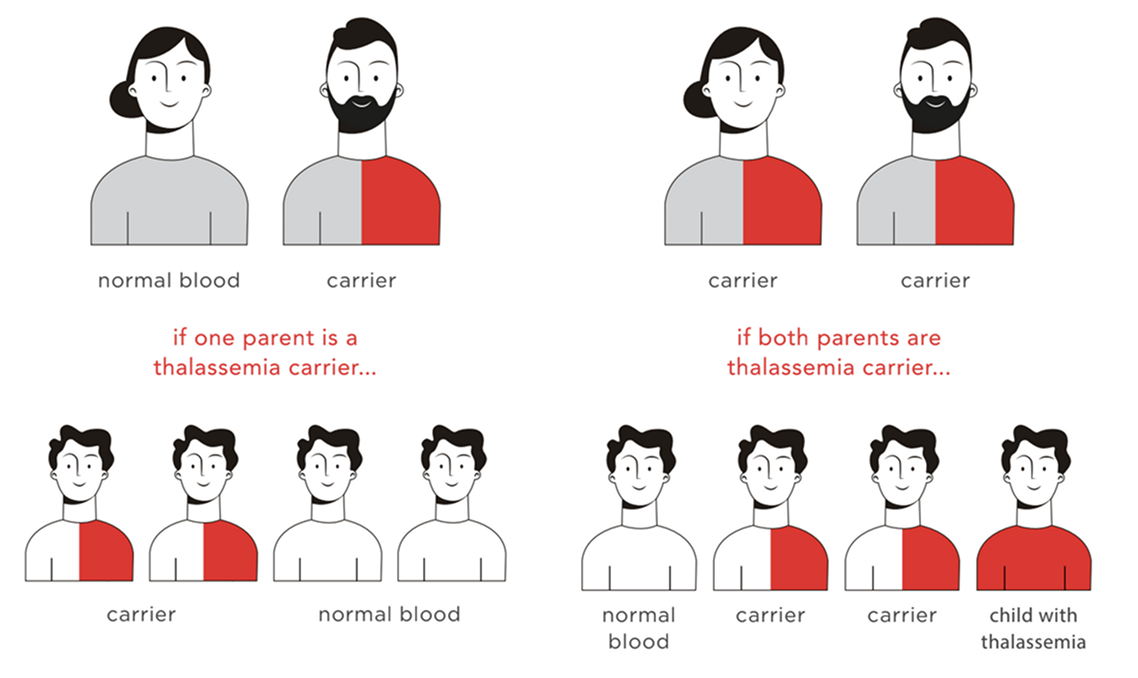
The Thala Test is a simple blood test that checks whether a person is a carrier of Thalassemia. Being a carrier does not mean you are sick or will ever need treatment. Most carriers live completely normal lives and often never know they carry the gene unless they get tested.
But here’s the important part: if both partners are carriers, there is a high chance that their child could be born with Thalassemia Major, a lifelong condition that requires regular blood transfusions and constant medical care. One small test, done at the right time, can prevent a lifetime of struggle for a child.Who should get tested?
The short answer: everyone.
Thalassemia does not belong to any one community, caste, religion, or income group. Anyone can be a carrier. That’s why we strongly believe that all individuals planning marriage or a family should get tested, regardless of background. Awareness should be universal, not selective.
Why we talk about the Thala Test so openly?
At The Wishing Factory, we’ve seen what life with Thalassemia looks like, not just in hospitals, but in homes, schools, and everyday routines. We believe prevention through awareness is one of the most powerful tools we have.
The Thala Test is not about fear; It’s about giving the next generation a healthier start. One test. One decision. A lifetime of impact.
Help the warriors survive and get special medical care throughout their lives.
WhatsApp us

Lorem Ipsum is simply dummy text of the printing and typesetting industry. Lorem Ipsum has been the industry’s standard dummy text ever since the 1500s, when an unknown printer took a galley of type and scrambled it to make a type specimen book. It has survived not only five centuries, but also the leap into electronic typesetting, remaining essentially unchanged. It was popularised in the 1960s with the release of Letraset sheets containing Lorem Ipsum passages, and more recently with desktop publishing software like Aldus PageMaker including versions of Lorem Ipsum